Spine-Related Musculoskeletal Conditions – Part 7 – Myelopathy
In this series, we have been reviewing spine-related musculoskeletal conditions that are frequently seen in dentists and surgeons. In this post, we will be looking at myelopathy.
Myelopathy
Definition: Myelopathy is damage to the spinal cord caused either by a traumatic injury or a chronic musculoskeletal condition. The term myelopathy generally refers to damage to the spinal cord, but may be used in reference to a handful of specific conditions, including:
Cervical Spondylotic Myelopathy: This is by far the most common form of myelopathy and involves the compression of the spinal cord in the cervical spine (neck). We will discuss cervical spondylotic myelopathy further below.
Thoracic Myelopathy: This occurs in the middle region of the spine. Typically, the spine gets compressed due to bulging or herniated discs, bone spurs, or spinal trauma.
Lumbar Myelopathy: This is a rare condition because the spinal cord typically ends in the upper section of the lumbar spine; however, the if the spinal cord is low-lying or tethered, it can be affected by this condition.
Cervical Spondylotic Myelopathy
Overview: Cervical spondylotic myelopathy is damage to the spinal cord due to spinal degeneration, most commonly in the form of spinal osteoarthritis. As the spinal cord is compressed (spinal stenosis) due to inflammation and osteophytes, it can cause damage to the spinal cord and lead to an array of neurological symptoms.
Causes: As discussed above, the inflammation and bone spurs (osteophytes) common to spinal osteoarthritis can exert pressure on the spinal cord and cause damage. Bulging and herniated discs and thickened ligaments can also contribute to myelopathy. In rarer cases an acute, traumatic injury to the neck can result in myelopathy.
Symptoms: Numbness, weakness, and/or tingling in the hands or arms, loss of balance, stiffness in the legs, and urinary urgency.
Diagnosis: A CT scan with a Myelogram is used to reveal indentations in the spinal fluid sac. In this procedure an opaque dye is injected into the spinal canal prior to the CT scan to create contrast and provide images of the spinal canal. This is done in conjunction with an MRI, which provides imaging of the spinal cord and nerve roots, as well as the intervertebral discs and spinal ligaments.
Treatment: Surgery to decompress the spinal cord and prevent further damage is the most common treatment for cervical spondylotic myelopathy. The precise nature of the surgery varies and depends on the severity of the condition and its location.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described below and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
References:
1. Spine-health, https://www.spine-health.com/.
2. Mayo Clinic, http://www.mayoclinic.org/.
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/.
5. WebMD, http://www.webmd.com/.
The Hartford Purchases Aetna’s Life And Disability Insurance Business for $1.45 Billion
Aetna has arranged to sell its group life and disability benefits to The Hartford for $1.45 billion dollars in cash. While group life and disability insurance were a small portion of Aetna’s business (about $2 million in premiums for 2016, compared to The Hartford’s $8.3 million in premiums at the end of the third quarter), this transaction will allow The Hartford the become second largest group life and disability insurer, behind MetLife. The Hartford will also obtain digital assets from Aetna, including absence, claims management, and data analytics systems, as well as a customer portal. And, following the sale, Aetna will offer The Hartford’s group life and disability products through Aetna’s sales force. The Hartford has also agreed to reinsure Aetna’s book of group life and disability insurance, on an indemnity basis.
While an Aetna press release states the two companies will work together to support their mutual customers, and the majority of Aetna’s 1,800 employees who support the acquired business will transfer to The Hartford, there are no details yet on how Aetna’s plans will be administered going forward, including for those already on claim.
The acquisition is expected to close in November 2017.
Sources:
Aetna, The Hartford Signs Agreement to Acquire Aetna’s U.S. Group Life and Disability Business, Oct. 23, 2017
The Hartford, The Hartford to Acquire Aetna’s U.S. Group Life and Disability Business, Special Presentation Webcast, Oct. 23, 2017
Japsen, Bruce, Aetna To Sell Group Life Business To Hartford for $1.4B, Oct. 23, 2017, 9:04 a.m.
Livingston, Shelby, Aetna to shed its life and disability insurance businesses for $1.5 billion, Modern Healthcare, Oct. 23, 2017
Otto, Nick, The Hartford to acquire Aetna’s life, disability business, Oct. 23, 2017, 2:39 p.m.,
Reuters, Hartford to buy Aetna US life and disability unit for $1.45 billion, CNBC, Oct. 23, 2017, 9:16 a.m.
Reuters, The Hartford to Buy Aetna Group Life, Disability Benefits Business for $1.45 Billion, Insurance Journal, Oct. 23, 2017
Spine-Related Musculoskeletal Conditions – Part 6 – Degenerative Disc Disease
In this series, we have been examining spine-related musculoskeletal conditions. In this post, we will be looking at degenerative disc disease.
Degenerative Disc Disease
Definition: Degenerative Disc Disease (DDD) is the breakdown in the size and cushioning of the intervertebral discs.
Overview: The name of the condition is actually somewhat of a misnomer – it is not actually a “disease”, but rather a condition that is characterized by the degeneration of the intervertebral discs over time. Over time, the pressure and wear of repetitive use can cause discs to lose some of their water content and volume, reducing their ability to cushion and insulate the vertebrae from one another.
Symptoms: The symptoms most commonly associated with DDD are chronic pain, weakness, numbness, and tingling in the extremities, and reduced flexibility in the spine. Not all people with intervertebral disc degeneration, however, experience pain or other symptoms. This is due to the fact that the degeneration of the discs, by itself, does not bring on the symptoms described above. However, as disc degeneration becomes more severe, it can lead to other conditions that bring on the symptoms people normally associate with DDD (e.g., pain, numbness and tingling, weakness, etc.). Some of the conditions commonly associated with DDD are spinal osteoarthritis, spinal stenosis, and foraminal stenosis.
Causes: Reduction in the size and cushioning of your discs is part of the normal process of aging, and magnetic resonance imaging (MRI) studies have shown that almost everyone over the age of 60 has degeneration of their intervertebral discs to some degree.[1] Not all people with disc degeneration have back pain or other symptoms – in fact, individuals with relatively mild disc degeneration may experience no symptoms whatsoever.
However, age is not the only factor in DDD. Deterioration of the intervertebral discs can be accelerated and exacerbated by other factors. The culprit in many severe cases of DDD is stress-related damage in the form of repetitive use, trauma, injury, poor posture, poor movement, and obesity. Among these, one of the most common factors is repetitive use. For example, the repetitive, static posture of a dentist during clinical procedures creates (1) compressive forces on the cervical discs due to neck flexion, and (2) compressive forces on the lumbar discs due to axial loading. When these compressive forces are applied year after year on a daily basis, the result can be an accelerated deterioration of the intervertebral discs.
Diagnosis: Diagnosis will generally begin with a physical exam in which the physician will perform a variety of tests to evaluate the patient’s strength and range of motion. If the physical tests indicate DDD, an MRI is typically ordered to measure the disc space and check for cartilage erosion.
Treatment: Because DDD can cause such a broad range of symptoms and subsequent conditions, the treatment options vary widely. Depending on the circumstances, treatment can range from conservative options such as physical therapy and anti-inflammatory medications to surgical intervention in the form of a discectomy, laminectomy, laminoplasty, or spinal fusion.
Our next and final post in this series will discuss myelopathy.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described below and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
[1] Degenerative Disc Disease, Arthritis Foundation, http://www.arthritis.org/about-arthritis/types/degenerative-disc-disease/
References:
1. Spine-health, https://www.spine-health.com/.
2. Mayo Clinic, http://www.mayoclinic.org/.
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/.
5. WebMD, http://www.webmd.com/.
SEAK Inc.’s 14th Annual Non-Clinical Careers for Physicians Conference, Oct. 21-22, 2017
SEAK, Inc.’s 14th Annual Non-Clinical Careers for Physicians Conference will be held on October 21 -22, 2017 in Chicago, Illinois. The conference is intended for physicians looking to explore careers outside the clinical setting.
Many doctors and dentists find themselves unable to practice, whether due to a disability, fatigue, burnout, loss of opportunity, wanting more control over their schedule, hope of financial gain, or just the desire to try a different career path or become an entrepreneur. The 375+ attendees at the conference will range from interns and residents to veteran physicians in their 70s. The conference aims to show physicians that switching to a non-clinical career is an opportunity with financial potential, and “is in fact a step forward, not a step backwards.” Attendees at the conference will network, meet with employers and recruiters, attend workshops and presentations and participate in one-on-one mentoring with physicians who have successfully made the transition to non-clinical careers. Several of the presenters have not only moved out of the clinical practice, but are also experienced life coaches dedicated to guiding other physicians into new careers. Sessions discuss opportunities for physicians with insurance companies, medical device companies, the pharmaceutical industry, contract research organizations, healthcare IT and medical informatics companies, and in education as well as in the consulting, medical administration, patient safety/quality, medical writing, and entrepreneurial fields.
Returning speakers include Gretchen M. Bosack, MD, who has transitioned to the Chief Medical Director of the Securian Financial Group and is also an accomplished public speaker; Rishi Anand, MD, who transitioned to the director of the Electrophysiology Laboratory at Holy Cross Hospital in Ft. Lauderdale, Florida, as well as serving as a medical legal consultant and expert witness, and a successful real estate investor; and Savi Chadha, MD, MPH, a medical science liaison with Tardis Medical Consultancy. The opening speaker, Philippa Kennealy, MD, MPH, CPCC, PCC, is president of The Entrepreneurial MD and the Physician Odyssey Program, where she helps physicians further their non-clinical careers.
Attorney Ed Comitz Addresses Disability Insurance Issues Faced By Professional Athletes
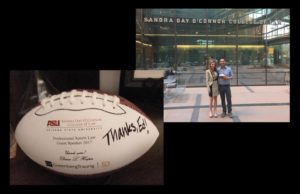
Ed Comitz was recently asked to speak at ASU’s Sandra Day O’Connor College of Law by Greenberg Traurig partner and leading sports agent, Dana Hooper, to address the key issues that professional athletes and their agents may encounter when dealing with disability insurance. Topics included the types of insurance coverage most often purchased by professional athletes, the tactics insurance companies use to deny athlete’s claims, and the importance of an attorney and/or agent’s role in the disability insurance context. The seminar also discussed the pros and cons of loss of value coverage for college athletes expected to go pro, and examined some of the challenges faced by injured athletes seeking to prove that a pre-draft injury caused them to fall in draft order and miss out on securing an upper-tier contract.
Mr. Comitz has represented high-earning professionals for nearly 25 years on the toughest insurance cases. As a result, he is intimately familiar with the disability insurance industry, and uses this knowledge to assist athletes from the “big four” sports (NFL, NBA, MLB, and NHL) seeking to negotiate favorable contracts with the premier, high-dollar insurance companies. He also advises professional athletes regarding the types of provisions to avoid in disability policies, the significance of the questions asked on disability insurance applications, and the importance of carefully reviewing insurance applications to ensure that they are accurate and do not provide the insurance company with any basis for voiding the policy, should a claim need to be filed later on down the road. When athletes are approaching free agency and intend to test the market, Mr. Comitz helps the athletes assess whether they need to purchase insurance to protect anticipated future income, should they suffer a serious injury before they are able to secure a contract with a new team. He also assists athletes with the legal issues that arise when an athlete is out for a few games, or an entire season, due to health concerns, and represents star athletes who have suffered a career-ending injuries and need to collect permanent disability benefits.
Subjective Conditions Limitation Provisions
In previous posts we’ve talked about mental health limitation provisions. In this post, we are going to discuss a similar type of provision: subjective symptom limitation provisions.
What are Subjective Symptom Conditions?
Insurance companies typically invoke subjective symptom limitation provisions when a claimant describes a disability or condition based upon self-reported symptoms, without producing objective medical evidence to back up the reported symptoms. This can occur in situations where there is no standard accepted medical test to confirm a diagnosis, or when tests do not return any confirming or conclusive results, or when a claimant has not properly developed his or her medical records and/or simply neglected to have objective testing done.
We most often see these types of limitations in ERISA policies, but they are becoming more and more common in individual policies. An example from an actual policy defines subjective symptoms as follows:

Some examples of conditions an insurance company might contend are encompassed by this provision include:
- Fibromyalgia
- Chronic Fatigue Syndrome
- Sleep Apnea
- Paresthesia/Dysesthesia
- Carpal Tunnel Syndrome
- Myofascial Pain Syndrome
- Lyme Disease
- Orthopedic Conditions
- Temporal Lobe Phenomenon
- Vertigo
- Migraine
- Tinnitus
- Irritable Bowel Syndrome
- Osteopathic and Rheumatoid Arthritis
- Generalized Pain
- Epstein-Barr Syndrome
- Valley Fever
Disability insurers also use these limitation provisions to argue that other conditions should be limited, even when there is some objective evidence. For example, a dentist suffering from a musculoskeletal condition might report to his or her doctor that he or she is experiencing neck pain, or lower back pain. The doctor might order an MRI, which might show that the dentist has some issues in his or her cervical or lumbar spine, but even with the MRI imaging, it can sometimes be difficult to pinpoint the precise cause of the symptoms that are being reported. Disability insurers know this and target these types of claims because, under a broad reading of the policy provision, they involve subjective reports of pain and the physical source of the pain cannot always be conclusively verified using tests.
Why is this provision important to know about?
These limitations typically cap disability benefits that will be paid out, generally at 12 to 24 months. After this mark has been reached, no additional disability benefits will be issued even if your symptoms continue and you cannot return to work. In other words, a disability insurance policy you thought would last for the maximum benefit period can end up being good for as little as a year.
Insurance companies want to avoid paying out disability claims and often construct policies in a manner that allows them to restrict or deny disability coverage. This can include hiding limitations at the end of a disability insurance policy or in a vaguely worded provision. It is not enough to simply look at a policy’s schedule page, because a limitation provision may actually be much broader limitation than you might think when you read “mental/nervous limitation” in your policy summary. Subjective condition limitation provisions are often combined with mental health and substance abuse limitation provisions, so it is easy for a policy holder to skip over this sort of provision when scanning through his or her policy, assuming that it only applies to mental health disorders or alcohol/addiction issues.
The Takeaway
When invoking these limitations, the insurance company is not denying that a claimant has an illness or even that it prevents a policyholder from working. Rather, the insurance company is seeking to take advantage of the limits of medical science and/or lack of agreement in the medical community regarding finding and establishing guidelines regarding conditions like the examples listed above. They then use the subjective condition provision to cast doubt on a claim and complicate the claim procedure. Often, they will use multiple in-house physicians to contradict a claimant’s own physician and medical records.
Fighting an insurance company’s decision to classify a condition as subject to this provision can be a costly and long process, and can turn into an expensive war of attrition that can often end in litigation. For these reasons, these types of claims must be handled with care from the start and require the assistance of a supportive doctor to properly document and treat the condition.
When purchasing a disability insurance policy, it is important to watch out for subjective symptom condition limitation provisions. Always be sure to read your disability insurance policy or potential policy carefully so that you understand the scope of the your protection.
Spine-Related Musculoskeletal Conditions – Part 5 – Disc Bulge, Disc Herniation, and Disc Protrusion
Our posts in this series have been reviewing spine-related musculoskeletal conditions that are frequently seen in dentists and surgeons. In this post, we will be looking at disc bulge, disc herniation, and disc protrusion.
Disc Bulge, Disc Herniation, and Disc Protrusion
Definitions:
- Disc Bulge: Protrusion of a spinal disc outside the vertebral body that has not fully ruptured through the disc membrane, known as the annulus.
- Disc Herniation: Protrusion of a spinal disc outside the vertebral body that has ruptured through the annulus, exposing a portion of the nucleus – the gel-like center of the disc.
- Disc Protrusion: A general term to describe any type of disc bulge or herniation, in which a portion of the disc protrudes beyond the vertebral body.
Overview: A number of terms are used to describe spinal disc pathology and the associated symptoms. To complicate matters further, there is not a clear consensus among medical professionals about the precise meaning of each term.
There are thirty-three vertebrae in the vertebral column of the human spine, twenty-four of which articulate and move. Between each of the vertebrae in the three articulating sections of the spine – the cervical, thoracic, and lumbar spine – there is an intervertebral disc. Each disc, composed of soft jelly-like center (nucleus) surrounded by a capsule of connective tissue (annulus), provides shock absorption and flexibility within the spine. When the protrusion puts pressure on the spinal cord or a nerve root, it can lead to a wide range of symptoms.
Symptoms: Symptoms will vary based on the location of the disc:
- Lumbar: Pain radiating down the leg (sciatica) is the most common symptom associated with a lumbar disc herniation. Weakness in the foot and difficulty when raising the big toe (foot drop) and numbness/pain on the top of the foot are also prevalent.
- Cervical: Pain, weakness, numbness, and tingling in the shoulder, arm, or hand depending on the location of the herniated disc.
Causes: Disc bulges are often the result of the normal process of aging, and by themselves may not cause any recognizable symptoms. Bad posture associated with frequent sitting or standing and occupational hazards such as repetitive bending or standing can accelerate the formation of disc bulges.
Disc herniation is often a progression in severity from a disc bulge. As discs wear down over time, they may degenerate and lose some of their water content. This condition, known as Degenerative Disc Disease, is discussed in greater detail below. As discs degenerate and degrade, they become more flexible and the annulus may be more susceptible to tearing or rupturing. Disc herniation can also be caused by traumatic, acute injuries such as a hard fall or blow to the back.
Diagnosis: Diagnosis of a herniated or bulging disc typically begins with a physical exam that tests the patient’s reflexes, muscle strength, walking ability, and sensory perception (light touches, pin pricks, etc.). If a protrusion is indicated by the physical test, imaging may be ordered in the form of X-rays, MRIs, CT scans, and/or Myelograms.
Treatment: Non-invasive treatment may include heat therapy, exercise, physical therapy, chiropractic treatment, therapeutic ultrasound, and medication. Epidural steroid injections may be considered as an intermediate treatment. For more severe cases, a microdiscectomy may be performed, typically in an outpatient setting. In this procedure, a small portion of bone and/or disc material is removed to relieve pressure on the affected nerve root.
Our next post will discuss degenerative disc disease.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described below and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
References:
1. Spine-health, https://www.spine-health.com/.
2. Mayo Clinic, http://www.mayoclinic.org/.
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/.
5. WebMD, http://www.webmd.com/.
Attorney Derek Funk Named in Top Valley Lawyers 2017

North Valley Magazine has named attorney Derek Funk as a Top Valley Lawyer for 2017. The list was compiled using a third-party attorney ranking system and showcases only 35 of the area’s best attorneys.
Spine-Related Musculoskeletal Conditions – Part 4 – Spondylolisthesis
In this series of blog posts, we have been reviewing spine-related musculoskeletal conditions. The next condition we will be looking at is spondylolisthesis.
Spondylolisthesis
Definition: Occurs when a vertebra (typically in the lumbar spine) slides forward over the vertebra beneath it.
Overview: The vertebrae in the spinal column are linked together by small joints (facets) that permit the spine to bend forward (flexion) and backward (extension) while limiting rotational movement. Spondylolisthesis occurs when a joint defect in the vertebrae (resulting from either a stress fracture or degeneration) permits one vertebra to slip forward on the one beneath it.
Spondylolisthesis is most common in the lower back, though in rare cases it can occur in the cervical spine. It most frequently occurs at the L4-L5 and L3-L4 levels of the lumbar spine.
There are two types of spondylolisthesis: isthmic spondylolisthesis (IS) and degenerative spondylolisthesis (DS). IS occurs when a stress fracture of a small bone called the pars interarticularis permits a vertebra to slip forward over the vertebra below it. IS is rare, and is most common in young children who participate in sports that put repeated stress on the lower back.
DS is far more common and most regularly occurs among people over the age of 50. DS is a result of the gradual breakdown of the intervertebral discs and the facet joints in the spine. As the discs lose volume, more stress and pressure is placed on the facet joints. As the facet joints begin to degrade under the increased wear and pressure, they may allow too much flexion and cause a vertebra to slip forward over the vertebral body below it.
The slippage can place direct pressure on the spinal cord (spinal stenosis) and on the nerve roots exiting the spinal column (foraminal stenosis).
Symptoms: Lower back pain, leg pain (especially “running down” the leg), and sciatic pain are common. Numbness or weakness often occurs in one or both legs. Leg/back pain that is worse when bending over or twisting is common, as is pain that is worse standing than sitting.
Causes: Degenerative disc disease is a common cause of spondylolisthesis. As we discussed above, when the intervertebral discs lose volume the spinal column becomes more compressed. Without the shock absorption of the discs, more pressure is exerted on the facet joints. This pressure and wear accelerates the degradation of the facets and allows for the increased flexion in the spine that can lead to vertebral slippage. As clinical dentistry has moved from a standing profession to a seated one, dentists are at a higher risk for lower back conditions like spondylolisthesis. Axial loading (the weight of the body compressing the spine vertically) on the lumbar spine is significantly higher in a seated position than it is standing.
Diagnosis: X-rays are used to determine whether or not a vertebra is out of place. If the displaced vertebra is putting pressure on the spinal cord or nerve roots, a CT scan may be ordered to identify the severity of the problem.
Treatment: As with many other conditions discussed in this series, conservative treatment may include some combination of physical therapy, exercise, strength training, manual manipulation, and medication. Epidural steroid injections are sometimes prescribed for those in severe pain. Spinal fusion surgery is sometimes used for severe pain that has not been successfully treated with less invasive treatment. Typically, a posterior fusion with a pedicle screw implementation is used, but a surgeon may also recommend a spinal fusion done from the font of the spine simultaneously.
Our next post in the series will examine disc bulge, disc herniation, and disc protrusion.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described below and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
References:
1. Spine-health, https://www.spine-health.com/.
2. Mayo Clinic, http://www.mayoclinic.org/.
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/.
5. WebMD, http://www.webmd.com/.
What is a Neuropsychological Evaluation? – Part 4
This is the last post in our series of posts about neuropsychological evaluations. We will conclude this series by discussing (1) why an insurance company would ask for an exam, and (2) how a neuropsychological evaluation can impact your disability claim.
Why Would My Insurer Ask for a Neuropsychological Evaluation?
Unfortunately, it is way too common for an insurer to look for ways to deny a disability claim, even in the face of strong medical proof of a disability. This can be especially true for conditions or disabilities that are more subjective than objective, or disabilities that include symptoms that cannot be definitely shown by commonly administered medical tests. An insurer intent on denying a disability claim may use Independent Medical Evaluations (IMEs), Functional Capacity Examinations (FCEs), Neuropsychological Evaluations, or a combination of these three exams, in its efforts to undercut a policyholder’s own doctor’s evaluation and medical records (particularly if the policyholder’s treating doctor is supportive of the claim and has clearly indicated that the policyholder should not return to work in their own occupation).
As we discussed previously, the limitations inherent in neuropsychological evaluations may lead to a conclusion that you are less cognitively impaired than you truly are, and/or a recommendation that you are able to return to work. Further, if the test is administered by a biased evaluator, results can be interpreted and manipulated in order to deny your disability claim.
What Can I Do?
First, make sure that your insurance company can actually require a neuropsychological examination under the terms of your disability insurance policy. Some policies include provisions requiring that claimants undergo “medical exams” or exams “conducted by a physician.” If your policy contained this sort of provision, you could potentially argue that the insurance company cannot require you to undergo a neuropsychological evaluation, since a neuropsychologist is not a physician, and this sort of exam is not strictly a “medical exam.”
If you must undergo the evaluation, there are several steps you can proactively take to prevent the examination from unfairly complicating or jeopardizing your disability claim, many of which are similar to steps you should take before an IME.
- Be sure to provide complete medical records.
- Carefully fill out any intake paperwork.
- Advise your medical team of the request for the evaluation.
- Take notes, including what questions were asked during the interview portion of the evaluation.
- Report back to your medical team after the test, especially regarding any negative effects, such as increased fatigue after the evaluation.
- Request a copy of the report.
It is important to note that neuropsychological evaluations are not inherently biased or a poor indicator of disability. In fact, they can actually be helpful in confirming your disability and demonstrate an impaired level of functioning that makes it impossible to return to work. In some instances, you may wish to undergo an exam with a truly independent examiner, either proactively or as a follow up to one ordered by your insurer. As with any new evaluation or course of treatment, you should carefully discuss this option with your current medical team and attorney, and obtain recommendations to a reputable evaluator.
Sources:
Atif B. Malike, MD; Chief Editor, et al., Neuropsychological Evaluation, Medscape, http://emedicine.medscape.com/article/317596-overview, updated May 18, 2017.
Neuropsychological Evaluation FAQ, University of North Carolina School of Medicine Department of Neurology, https://www.med.unc.edu/neurology/divisions/movement-disorders/npsycheval
Kathryn Wilder Schaaf, PhD, et al, Frequently Asked Questions About Neuropsychological Evaluation, Virginia Commonwealth University Department of Physical Medicine and Rehabilitation, https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwir3pKk__fUAhUBEmMKHenkDzsQFggoMAA&url=http%3A%2F%2Fwww.tbinrc.com%2FWebsites%2Ftbinrcnew%2Fimages%2FNeuropsych_FAQ.pdf&usg=AFQjCNG0Mv3o17ZrNmXuDN5ITUIh4fWYtA&cad=rja
What is a Neuropsychological Evaluation? – Part 3
Our previous posts in this serious have examined what a neuropsychological evaluation is and how these exams are conducted. In this post we’ll be talking about some of the limitations associated with these types of exams.
How Reliable Are Neuropsychological Evaluations?
As we explained in previous posts, neuropsychological evaluations seek to provide information about the brain and behavior through the use of established, standardized tests that produce quantitative data. This data can then be used to confirm and back up a subject’s reports of cognitive impairment.
These evaluations can serve several purposes, such as corroborating the cognitive effects of a disability, or outlining a subject’s limitations in his or her daily life (including the inability to return to one’s own occupation). For example, an evaluation might show that a dentist with a head injury has impaired motor skills and visuospatial processing abilities that make it unsafe for the dentist to continue treating patients. In this sense, an evaluation can provide data that can lend further support to a disability claim, but wouldn’t necessarily show up on an MRI or the results from other types of medical testing.
However, while these evaluations can be useful, they also have certain limitations that are important to consider. As with Functional Capacity Evaluations (FCEs) the examination is truly just a snapshot—the data is based on your functioning on a specific day, for a limited amount of time, in a quiet and controlled testing room.
Generally, findings indicate that performance on tests of motor function, speed of cognitive processing, cognitive flexibility, complex attention, and memory are related positively to real-word success. However, some argue that these exams do not adequately take into account the fact that, in the real world, several executive functions (such as recognizing a task must be completed, starting a task, switching tasks, making needed changes, finishing a task, etc.) can occur simultaneously. Further, the administered test may not indicate whether a subject was mentally exhausted after the test,[1] and thus may not provide any insight into whether the subject is able to sustain the same demonstrated level of executive functioning day in and day out.
While the administered tests are designed to be objective and produce results that can be extrapolated across populations, this is not always possible. While a subject’s results should be compared with both population-based norms as well as specific patient populations for strengths and weaknesses, there can be gaps in normative data for certain age, educational, and intellectual ranges.[2] This can be especially true for minority populations.[3] Along these same lines, an evaluator may not take into account norms specific to doctors, or a doctor’s need for higher performance on certain tests (e.g. those for sensory-perceptual functions), when assessing whether a return to work is possible.
Excessive fatigue, medications, lack of motivation (sometimes due to depression), emotional distress, severe psychiatric conditions, serious medical complications, and illicit substances can also all impact the reliability of an evaluation.
Additionally, as we’ve discussed before in the context of Independent Medical Examinations (IMEs), a neuropsychological examiner selected by an insurance company may be presented as independent, but may not truly be so. An examiner selected and paid for by a disability insurer may be more likely to report that a subject is “malingering,” trying to influence a test’s outcome, or not putting forth a true effort.
In our next post, we will further explain why an insurer might require a neuropsychological evaluation, and how these exams can impact a disability claim.
[1] Atif B. Malike, MD; Chief Editor, et al., Neuropsychological Evaluation, Medscape, http://emedicine.medscape.com/article/317596-overview, updated May 18, 2017.
[2] Id.
[3] Id. (citing Decker SL, Schneider WJ, Hale JB, Estimating Rates of Impairment in Neuropsychological Test Batters: A Comparison of Quantitative Models, Arch. Clin. Neuropsychol. 2011 Dec 15 [Medline].
Sources:
Atif B. Malike, MD; Chief Editor, et al., Neuropsychological Evaluation, Medscape, http://emedicine.medscape.com/article/317596-overview, updated May 18, 2017.
Neuropsychological Evaluation FAQ, University of North Carolina School of Medicine Department of Neurology, https://www.med.unc.edu/neurology/divisions/movement-disorders/npsycheval
Kathryn Wilder Schaaf, PhD, et al, Frequently Asked Questions About Neuropsychological Evaluation, Virginia Commonwealth University Department of Physical Medicine and Rehabilitation, https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwir3pKk__fUAhUBEmMKHenkDzsQFggoMAA&url=http%3A%2F%2Fwww.tbinrc.com%2FWebsites%2Ftbinrcnew%2Fimages%2FNeuropsych_FAQ.pdf&usg=AFQjCNG0Mv3o17ZrNmXuDN5ITUIh4fWYtA&cad=rja
Spine-Related Musculoskeletal Conditions – Part 3 – Stenosis
In this series, we have been looking at spine-related musculoskeletal conditions that many dentists and surgeons suffer from. In this post, we will be looking at spinal and foraminal stenosis.
Cervical Spinal Stenosis:
Definition: The narrowing of the spinal canal in the cervical vertebrae, often due to inflammation of the surrounding cartilage and tissue.
Overview: The spinal canal is formed by the hollow spaces in the middle of the vertebrae, which form a protective tunnel for the spinal cord to pass through the spinal column. Cervical spinal stenosis is a progressive and potentially dangerous condition that occurs when inflammation narrows the cervical spinal canal. The narrowing of this already tight space can result in direct pressure on the spinal cord, leading to a number of neurological complications. Cervical spinal stenosis can be crippling if the spinal cord becomes damaged.
Symptoms: Symptoms usually develop gradually over time and can include numbness, weakness, tingling in neck, shoulders, arms, hands, or legs, as well as intermittent, sharp pain in the arms and legs, especially when bending forward. Deterioration of fine motor skills and issues with gait and balance can also occur. In more severe cases, bladder and bowel issues may develop.
Causes: Though in rare cases cervical spinal stenosis is a congenital condition, it often results from inflammation due to other spinal conditions, such as spinal osteoarthritis, degenerative disc disease, and disc bulging.
Diagnosis: A combination of X-ray, MRI, and computed tomography (CT) scans may be used to diagnose spinal stenosis. Blood tests may be used to eliminate other diseases such as multiple sclerosis and vitamin B12 deficiency.
Treatment: Conservative, non-invasive treatments may include exercise, physical therapy, and activity modification. Medications may include anti-inflammatory drugs, narcotic pain medication, muscle relaxers, and epidural steroid injections. In more severe cases, several surgical options exist, dependent upon the particular characteristics of the patient’s condition:
Anterior cervical discectomy/corpectomy with fusion (ADCF): The spine is accessed through the front of the patient’s neck, the disc is removed from between the two vertebrae, and the vertebrae are then fused together to stabilize the spine.
Laminectomy: This is a “decompression” surgical procedure performed to relieve pressure on the spinal cord. In this surgery, the lamina (the rear portion of the vertebra covering the spinal canal) is removed from the affected vertebra to enlarge the spinal canal and decrease pressure on the spinal cord.
Interspinous Process Spacers: In this procedure, small metal spacers are surgically placed between the vertebrae to restore the spacing typically created by a healthy disc. This procedure is typically reserved for individuals with foraminal stenosis, however, and has only had limited effectiveness with patients suffering from spinal stenosis.
Foraminal Stenosis
Definition: Compression of the nerve roots connected to the spinal cord, caused by the narrowing of the passageway through which the nerves exit the spinal column.
Overview: The nerve roots branching off the spinal cord to other parts of the body exit the spinal column through small openings on the sides of the vertebrae called a foramen. This space can become clogged or narrowed due to a number of spine-related conditions. The narrowing or partial obstruction of the foraminal canal caused by one of these conditions can put pressure on the nerve roots emerging from the spinal column, and may lead to an array of neurological symptoms that get progressively worse over time.
Symptoms: Tingling, numbness, or weakness in the feet or hands. Local pain in the extremities. “Pins and needles” or burning sensation. Intermittent neck or back pain.
Causes: Bulging or herniated discs may obstruct the foraminal canal, putting pressure on the nerve roots. It can also be caused by spinal osteoarthritis, osteophytes, and spondylolisthesis. Dentists are susceptible to foraminal stenosis, as they often hold their necks in extended positions.
Diagnosis: A CT scan and a Myelogram are used to diagnose foraminal stenosis. A Myelogram is an X-ray in which an opaque dye (which shows up on the X-ray) is injected into the sac around the nerve roots. The dye moves through the foramina, allowing the doctor to see the degree to which the foramen is narrowed or obstructed.
Treatments: Conservative treatments may include physical therapy, stretching and strength training, and oral pain-relieving medication. Corticosteroid injections are an option for more severe cases to reduce inflammation and pain. In extreme cases, a surgical procedure known as a foraminotomy may be used to remove the bone spur or disc material that is putting pressure on the nerve root as it exits the spinal column through the foramen.
Our next post in this series will discuss spondylolisthesis.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described below and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
References:
1. Spine-health, https://www.spine-health.com/.
2. Mayo Clinic, http://www.mayoclinic.org/.
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/.
5. WebMD, http://www.webmd.com/.
Spine-Related Musculoskeletal Conditions – Part 2 – Spinal Osteoarthritis
In the first part of this series, we discussed the fact that dentists and surgeons often suffer from musculoskeletal conditions. In the remaining posts in this series, we will be looking at particular musculoskeletal conditions, starting with spinal osteoarthritis.
Spinal Osteoarthritis
Definition: Spinal osteoarthritis is also known as degenerative joint disease. It is a breakdown of the cartilage in the facet joints, which link together the spine’s vertebrae.
Overview: At the top and bottom of each vertebra is a small pair of joints called facets. Facets connect the vertebrae in order to restrict movement in certain directions and to allow the spine to move as one fluid unit. The surfaces of the facets, like any other joint in the human body, are covered by a lubricating cartilage which allows them to operate smoothly and with little friction.
When the cartilage protecting the facets degrades or wears down, the bony surfaces of the facets rub against each other. This can cause inflammation, severe pain, and the formation of osteophytes (bone spurs) on or around the joint surfaces. It may also cause numbness and/or weakness in the legs and arms as a result of contact between the vertebrae and the nerves leaving the spinal cord.
Symptoms: Neck pain and stiffness. Severe pain may radiate down into shoulders and up the neck. Weakness, numbness, or tingling in the fingers, hands, and/or arms are also often present. Usually back discomfort is relieved when a person is lying down. Studies have also linked anxiety and depression to osteoarthritis.[1]
Causes: Spinal osteoarthritis frequently occurs in conjunction with degenerative disc disease. As the discs between the vertebrae in the spinal column degrade and decrease in volume, the increased pressure and contact between the facet joints can cause an accelerated degradation of the joint cartilage.
Repetitive strain or stress on the spine, often due to poor posture, to is a common cause of spinal osteoarthritis. People with jobs requiring repetitive movements and strained positions are considered to be at greater risk for conditions like spinal osteoarthritis; however, injury or trauma to a joint or a genetic defect involving cartilage are also causes. Dentists are at a higher risk than many other professions to develop this condition due to the awkward, static postures they must maintain.
Diagnosis: X-rays may be used to identify loss of cartilage, bone spurs, and bone damage. Magnetic resonance imaging (MRI) may be used to analyze the intervertebral discs and the nerves exiting the spinal column.
Treatment: Conservative, non-invasive treatment plans may include some combination of heat/cold therapy, medication, physical therapy, strength training, and stretching. In more severe cases, a surgical treatment such as spinal fusion is utilized.
Our next post in this series will examine spinal stenosis, another common cause of neck and back pain.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described below and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
[1] Sharma, A., et. al, Anxiety and depression in patients with osteoarthritis: impact and management challenges, Open Access Rheumatology: Research and Reviews 2016:8 (2016).
References:
1. Spine-health, https://www.spine-health.com/.
2. Mayo Clinic, http://www.mayoclinic.org/.
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/.
5. WebMD, http://www.webmd.com/.
What is a Neuropsychological Evaluation? – Part 2
In our last post, we looked at what a neuropsychological evaluation is, and how it can be used as a tool to identify cognitive impairments. In this post we will talking about how a neuropsychological evaluation works in more detail.
What Can I Expect During a Neuropsychological Evaluation?
A neuropsychological evaluation will generally consist of (1) a review of your medical and other records (this could include your disability insurance claim file); (2) an interview with you and sometimes another person such as a family member or caregiver who knows you well, (especially if your disability impacts your ability to self-report); and (3) the administration of tests that measure both your mood and abilities.
The evaluation will typically begin with an interview and then proceed to testing. The tests will be both written and oral, and vary in length and complexity. Often the tests will be administered by a specially trained technician, or a psychometrist. The typical evaluation takes between two to five hours to complete, but can stretch up to eight hours and/or be split into two sessions. Conditions such as fatigue or motor impairments can slow down the process.
The results will generally be presented in a report that includes a summary of the tests conducted, a summary of your key medical and personal history, your current issues (i.e. the reason the neuropsychological exam was requested), the results of the testing, how these results compare to other people with your background, and a list of recommendations. As explained previously, these recommendations can help indicate the need for additional treatment, suggest treatment options, and/or provide information on cognitive deficiencies and resulting physical and mental limitations.
The evaluation is designed to assess your knowledge, functioning, and skills at the time of the exam. Because of this, it is not the sort of test that you would “study” for, in the same sense that you would study for, say, an academic exam. However, if you are going to be undergoing a neuropsychological exam, evaluators typically recommend that you:
insert
- Get a good night’s sleep
- Put forth your best effort
- Provide a list of all medications and take all medication as normally scheduled, unless instructed otherwise
- Bring a friend or family member if you have trouble relating information about your history (for the interview portion of the examination)
- Make sure the evaluator has access to your medical records
- Do not consume alcohol or other illicit substances within the 24 hours prior to the evaluation
- Notify the examiner of excessive fatigue, psychological distress, or frequent changes in your ability to move
Our next posts in this series will address the reliability of neuropsychological examinations and why your disability insurance company may ask for one.
Sources:
Atif B. Malike, MD; Chief Editor, et al., Neuropsychological Evaluation, Medscape, http://emedicine.medscape.com/article/317596-overview, updated May 18, 2017.
Neuropsychological Evaluation FAQ, University of North Carolina School of Medicine Department of Neurology, https://www.med.unc.edu/neurology/divisions/movement-disorders/npsycheval
Kathryn Wilder Schaaf, PhD, et al, Frequently Asked Questions About Neuropsychological Evaluation, Virginia Commonwealth University Department of Physical Medicine and Rehabilitation, https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwir3pKk__fUAhUBEmMKHenkDzsQFggoMAA&url=http%3A%2F%2Fwww.tbinrc.com%2FWebsites%2Ftbinrcnew%2Fimages%2FNeuropsych_FAQ.pdf&usg=AFQjCNG0Mv3o17ZrNmXuDN5ITUIh4fWYtA&cad=rja
What is a Neuropsychological Evaluation? – Part 1
We’ve talked before about how your insurance company may require you to undergo an independent medical examination (IME) by a physician of their choosing and how they may also ask for a Functional Capacity Evaluation (FCE).
Neuropsychological evaluations are another tool insurers utilize when investigating disability claims. A neuropsychological evaluation is also something that a claimant filing a disability claim may choose to undergo independently, to provide additional proof of his or her disability. In this series of posts, we will be talking about what a neuropsychological evaluation is, what to expect during an examination, and how an exam could affect your disability claim.
What is a Neuropsychological Evaluation?
Neuropsychology is the study of the relationship between the brain and behavior. A neuropsychological evaluation is a method of testing where a neuropsychologist seeks to obtain data about a subject’s cognitive, behavioral, linguistic, motor, and executive functioning in order to identify changes that are, often, the result of a disease or injury. The evaluation can lead to the diagnosis of a cognitive deficit or the confirmation of a diagnosis, as well as provide differential diagnoses.
Neuropsychological evaluations are most often associated with conditions that exhibit cognitive dysfunctions, such as:
- Multiple sclerosis
- Alzheimer’s
- Epilepsy or seizures
- Psychological and mental health disorders
- Chronic pain
- Head injuries
- Stroke
- Parkinson’s disease
- Neurodegenerative diseases
- Side effects of medication
Conditions such as those enumerated above often have symptoms that vary person by person, and the amount of cognitive impairment can often not be fully assessed by other diagnostic tools such as an MRI, or a traditional psychological evaluation.
Neuropsychological tests are standardized tests that are given and scored in a similar manner each time they are used. The tests are designed to evaluate the following:
- Intellectual Functioning
- Academic Achievement
- Language Processing
- Visuospatial Processing
- Attention/Concentration
- Verbal Learning and Memory
- Executive Functions
- Speed of Processing
- Sensory-Perceptual Functions
- Motor Speed and Strength
- Motivation
- Personality
There are many different accepted tests for each domain listed above. Accordingly, an examiner will likely not perform every test, but rather select tests from each category that will best evaluate the particular question posed by the referrer.
The goal of these neuropsychological tests is to produce raw data. The results are then evaluated by comparing test scores to healthy individuals of a similar background (age, education, gender, ethnic background, etc.) and to expected levels of cognitive functioning. The data is then interpreted by the neuropsychologist, and perhaps other providers, to determine the strengths and weaknesses of the subject’s brain, provide suggestions for potential treatment options, set a standard for any future testing, evaluate a course of treatment, make recommendations on steps and modifications that can improve daily living, and evaluate whether a subject can return to work with or without modifications.
In our next post we will go look at what you can expect during a neurospychological evaluation.
Sources:
Atif B. Malike, MD; Chief Editor, et al., Neuropsychological Evaluation, Medscape, http://emedicine.medscape.com/article/317596-overview, updated May 18, 2017.
Neuropsychological Evaluation FAQ, University of North Carolina School of Medicine Department of Neurology, https://www.med.unc.edu/neurology/divisions/movement-disorders/npsycheval
Kathryn Wilder Schaaf, PhD, et al, Frequently Asked Questions About Neuropsychological Evaluation, Virginia Commonwealth University Department of Physical Medicine and Rehabilitation.
What is a Neuropsychological Evaluation? – Part 1
We’ve talked before about how your insurance company may require you to undergo an independent medical examination (IME) by a physician of their choosing and how they may also ask for a Functional Capacity Evaluation (FCE).
Neuropsychological evaluations are another tool insurers utilize when investigating disability claims. A neuropsychological evaluation is also something that a claimant filing a disability claim may choose to undergo independently, to provide additional proof of his or her disability. In this series of posts, we will be talking about what a neuropsychological evaluation is, what to expect during an examination, and how an exam could affect your disability claim.
What is a Neuropsychological Evaluation?
Neuropsychology is the study of the relationship between the brain and behavior. A neuropsychological evaluation is a method of testing where a neuropsychologist seeks to obtain data about a subject’s cognitive, behavioral, linguistic, motor, and executive functioning in order to identify changes that are, often, the result of a disease or injury. The evaluation can lead to the diagnosis of a cognitive deficit or the confirmation of a diagnosis, as well as provide differential diagnoses.
Neuropsychological evaluations are most often associated with conditions that exhibit cognitive dysfunctions, such as:
- Multiple sclerosis
- Alzheimer’s
- Epilepsy or seizures
- Psychological and mental health disorders
- Chronic pain
- Head injuries
- Stroke
- Parkinson’s disease
- Neurodegenerative diseases
- Side effects of medication
Conditions such as those enumerated above often have symptoms that vary person by person, and the amount of cognitive impairment can often not be fully assessed by other diagnostic tools such as an MRI, or a traditional psychological evaluation.
Neuropsychological tests are standardized tests that are given and scored in a similar manner each time they are used. The tests are designed to evaluate the following:
insert
- Intellectual Functioning
- Academic Achievement
- Language Processing
- Visuospatial Processing
- Attention/Concentration
- Verbal Learning and Memory
- Executive Functions
- Speed of Processing
- Sensory-Perceptual Functions
- Motor Speed and Strength
- Motivation
- Personality
There are many different accepted tests for each domain listed above. Accordingly, an examiner will likely not perform every test, but rather select tests from each category that will best evaluate the particular question posed by the referrer.
The goal of these neuropsychological tests is to produce raw data. The results are then evaluated by comparing test scores to healthy individuals of a similar background (age, education, gender, ethnic background, etc.) and to expected levels of cognitive functioning. The data is then interpreted by the neuropsychologist, and perhaps other providers, to determine the strengths and weaknesses of the subject’s brain, provide suggestions for potential treatment options, set a standard for any future testing, evaluate a course of treatment, make recommendations on steps and modifications that can improve daily living, and evaluate whether a subject can return to work with or without modifications.
In our next post we will go look at what you can expect during a neurospychological evaluation.
Sources:
Atif B. Malike, MD; Chief Editor, et al., Neuropsychological Evaluation, Medscape, http://emedicine.medscape.com/article/317596-overview, updated May 18, 2017.
Neuropsychological Evaluation FAQ, University of North Carolina School of Medicine Department of Neurology, https://www.med.unc.edu/neurology/divisions/movement-disorders/npsycheval
Kathryn Wilder Schaaf, PhD, et al, Frequently Asked Questions About Neuropsychological Evaluation, Virginia Commonwealth University Department of Physical Medicine and Rehabilitation.
Spine-Related Musculoskeletal Conditions – Part 1 – Spondylosis
Living with a spine-related condition can be scary and overwhelming. Unfortunately, the complex nature of the spine and the nervous system can often make the search for answers a frustrating and demoralizing endeavor. In this series of posts we are going to talk about several spine-related musculoskeletal conditions, many of which are frequently diagnosed in dentists, surgeons, and other physicians.
If you are suffering from a spine-related condition, you have likely visited not only your primary care physician, but also a physical therapist, a chiropractor, a neurologist, an orthopedic surgeon, and/or a pain management doctor. It’s common for those suffering from a musculoskeletal condition to hear several different terms to describe a set of symptoms, be given multiple explanations for what is causing their pain, and be given a variety of (often conflicting) treatment recommendations.
Dentists and physicians in certain surgical specialties are particularly susceptible to spine-related musculoskeletal conditions, which are among the top reasons insureds file disability claims. The forward-flexed, static posture that dentists and surgeons must maintain to perform procedures can lead to the overuse and repetitive strain of the neck and back, and contribute to the development of a litany of musculoskeletal conditions. One study showed that 62% of the general population present musculoskeletal work-related pain, and this increased to 93% when the sample population was made up entirely of dentists.[1] Unfortunately, although one often thinks of spinal and back injuries occurring later in life after years of strain, chronic musculoskeletal pain is experienced by many dentists by their third year of dental school.[2]
We’ve created this series of blog posts as a resource to help clear up some of the confusion surrounding the common terms used to refer to spine-related musculoskeletal conditions. For each term we’ll provide a definition, overview, list of common symptoms, causes, methods of diagnosis, and common treatments. In this post, we’re going to briefly look at spondylosis, and then in later posts we will take a more in depth look at some other spine-related conditions.
Spondylosis
Definition: This is an umbrella term used to broadly describe degeneration in the spine. Some doctors may use it interchangeably with spinal osteoarthritis. Spondylosis is a descriptive term rather than a clinical diagnosis – it is used to describe anyone suffering from both pain and spinal degeneration. If your doctor uses this term to describe your condition, you may want to your physician for a more specific diagnosis.
These posts are for informative purposes only and should not be used as a substitute for consultation with and diagnosis by a medical professional. If you are experiencing any of the symptoms described above and have yet to consult with a doctor, do not use this resource to self-diagnose. Please contact your doctor immediately and schedule an appointment to be evaluated for your symptoms.
[1] Dias, Ana Giselle Aguiar, et. al, Prevalence of repetitive strain injuries/work related musculoskeletal disorders in different specialties of dentists, RGO, Rev. Gauch. Odontol. Vol. 62 no. 2, Campinas Apr./June 2014, http://dx.doi.org/10.1590/1981-8637201400020000042714 (citing Regis Filho GI, Michels G, Sell I. Lesões por esforços repetitivos/distúrbios osteomusculares relacionados ao trabalho em cirurgiões-dentistas. Rev Bras Epidemiol. 2006;9(3):346-59, http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1415-790X2006000300009&lng=en).
[2] Kristina Lynch, My back is hurting my practice, Part I, AGD Impact, Feb. 2006.
References:
1. Spine-health, https://www.spine-health.com/
2. Mayo Clinic, http://www.mayoclinic.org/
3. The Neurological Institute of New York,
http://columbianeurology.org/about-us/neurological-institute-new-york.
4. John Hopkins Medicine, http://www.hopkinsmedicine.org/
5. WebMD, http://www.webmd.com/
Do I Have to Keep Paying Premiums Even Though I’m Disabled?
If you are thinking about filing a disability claim, you are likely wondering whether you will be able to meet your monthly expenses if you’re no longer able to work. You may have made a list of your necessary expenses, and likely included your disability insurance premium payments on that list, as your agent likely told you that your policy would lapse and you would lose your coverage if you missed a premium payment. At this point, you probably started to wonder whether you still have to keep paying the premium after you file the disability claim, and if so, for how long?
The answer depends on the specific terms of your policy. The paragraph that you’ll want to look for when you’re reviewing your policy is typically titled “waiver of premium,” but some policies address waiver of premiums as part of a larger section of the policy that discusses premiums more generally.
How Do Waiver of Premium Provisions Work?
Generally speaking, waiver of premium provisions state that your disability insurance company cannot charge premiums during periods of time when you are disabled. A waiver of premium provision typically will also require your insurance company to reimburse you for premiums you have previously paid during your period of disability (i.e. the premiums that you paid while the insurance company was investigating your claim).
Waiver of premium provisions are included in most disability insurance policies. If you are considering purchasing a policy that does not include a waiver of premium provision, you may have the option to purchase a waiver of premium rider.
Here is an example of a waiver of premium provision from an actual disability insurance policy.
————————————————————————————————————————————
Waiver of Premium Benefit
We will waive Premiums of this Policy from the date of Total Disability after the later of:
- 90 consecutive days of Total Disability, or
- The end of the Elimination Period.
When we approve the Waiver of Premium, We will refund any Premiums paid from the first day of Total Disability. Waiver of Premium will continue while You are receiving a Total or Partial Disability Benefit of this Policy or a Rider. When You are no longer eligible for Waiver of Premiums, You must resume payment of Premiums to keep Your Policy in force.
————————————————————————————————————————————
Under this policy, the waiver of premium provision requires you to pay premiums either for 90 consecutive days after you become disabled, or until the end of the elimination period (the elimination period is the number of days you must be disabled before you are entitled to benefits, and is usually noted on the first few pages of a policy).
So, for example, under this policy, once you have been disabled for 90 consecutive days, you no longer would have to pay premiums (at least until you recover from your disability, or your insurer terminates your benefits). You also would receive a refund of any premiums that you paid for any period prior to your date of disability.
Notably, the waiver of premium provision above also requires you to be receiving benefits for the waiver to apply. This is significant because, depending on the terms of your policy, in some cases you could be disabled but not receiving benefits. For instance, your policy might have a foreign residency limitation that prevents you from receiving benefits if you are living in another country, even if you remain disabled. In such a case, you might have to resume paying premiums until you returned to the United States in order to keep your coverage in force.
The Takeaway
Timely and proper payment of premiums is critical, as a failure to pay premiums can result in you losing your disability coverage completely. It is important to read your disability insurance policy carefully so that you have a clear understanding of when you are required to pay premiums, and when you are entitled to a refund of past premiums.
Most insurance companies will provide you with written confirmation that premiums have been waived, and it is best to keep paying your premiums until you receive this written confirmation, even if you think that you no longer have an obligation to pay premiums under the terms of your policy. If you have questions about whether your insurance company should have waived and/or refunded premiums under the terms of your policy, an experienced disability insurance lawyer can review your policy and explain your rights and obligations under your particular policy.
Don’t Owe Your Insurer Money – Be Aware of Overpayment Provisions
In previous posts, we’ve discussed how insurance companies typically place caps on how much disability coverage a policyholder can receive. For physicians and dentists, this typically results in monthly disability benefit amounts that are lower (and sometimes much lower) than the monthly income you would bring in if you were still able to practice.
In some cases, policyholders are able to supplement their income by working in another field, but this is only possible if your disability insurance policy allows you to work in another occupation. Alternatively, your policy could contain a “no work” provision, which would foreclose this as an option. And some newer policies even require you to be working in order to collect disability benefits, so you don’t have a choice–you must find another job if you want to receive your disability benefits each month.
If you are not able to work in another occupation, due to the nature of your disabling condition and/or the contractual terms of your policy, you may be placed in a position where you must either cut expenses, find another source of income, or both. If you find yourself in this unenviable position, or you are planning ahead and contemplating what you might do in this sort of situation, you will want to keep in mind that some policies–particularly employer-sponsored plans–can contain offset provisions, which allow the insurance company to reduce your monthly disability benefit if you receive additional income from certain enumerated sources.
What Types of “Other Income” Can Be Offset?
There are many types of income that your disability insurer might include in an offset provision. Some examples include:
- Social Security benefits;
- Pension plans;
- Sick leave or a salary continuation plan of an employer;
- Income from other disability insurance policies;
- Retirement benefits funded by an employer;
- Workers’ compensation;
- Partnership or shareholder distributions; or
- Amounts paid because of loss of earning capacity through settlement, judgment, or arbitration.
The list above is by no means exhaustive and, again, you should carefully review your disability insurance policy for its specific list of offsets.
What are Overpayment Provisions?
If your disability insurance policy contains an offset provision, it will also likely contain an overpayment provision. In most instances, if your policy contains an offset provision, your insurer will be able collect information about your income from other sources prior to issuing the disability benefit, and calculate the amount due accordingly. However, in some cases this is not possible.
For example, say you applied for Social Security disability benefits. In some cases, it can take several years before a Social Security determination is made. Then, at that point, if your disability claim was approved, you would receive a lump sum of benefits covering the time period from the date of disability you reported to the date your claim was approved.
This is where the overpayment provision kicks in. If your policy has an overpayment provision, upon learning of the lump sum payment from Social Security, your insurer could potentially require you to pay the entire lump sum of benefits back to your insurance company (depending on the terms of your policy). This is because the lump sum payment represents several monthly payments you would have received over the relevant time frame. If your insurer paid the full monthly disability benefit for those months and your policy has an offset provision, your insurer will likely ask for the Social Security benefits as payment for the amounts that should have been offset each month over that time period.
What Happens if You Cannot Pay Back the Overpayment in a Lump Sum?
If you are not in a position to pay back an overpayment in a lump sum, your disability insurer will seek to collect the overpayment amount in other ways. One way is reducing and/or withholding future disability benefits until the full amount of the overpayment has been recouped by the insurer. Your insurer may also work out a payment plan with you, initiate collection efforts against you and/or file suit to recover the overpayment.
The Takeaway
Offset and overpayment provisions can be particularly devastating if you are caught unaware and find yourself with considerably less income than expected, or an obligation to repay a large sum to your insurer. When selecting a disability insurance policy, you should try and avoid these types of provisions if at all possible. If you already have a policy, you should read it carefully, so that you are fully aware of any offsets that could occur and any overpayments that you could potentially be responsible for under the terms of your disability policy.
Can You Move Out of the Country and Still Receive Disability Benefits?
The answer depends on what your disability policy says. Many people don’t realize that their disability insurance policy may limit their ability to receive disability benefits if they move out of the country. If you’ve ever wondered why claims forms ask for your updated address, one of the reasons might be that your disability policy contains a foreign residency limitation, and your insurance company is trying to figure out if they can suspend your disability benefits.
Foreign residency limitations allow disability insurance companies to stop paying benefits under your policy if you move out of the country. These limitations may be especially relevant if you have dual citizenship, you want to visit family living abroad, or you plan to obtain medical care in another country. A foreign residency limitation may also affect you if your disability insurance policy allows you to work in another occupation and you have a job opportunity in another country that you want to pursue. For instance, if you are a dentist and can receive disability benefits while working in another occupation, your insurance company may suspend your benefits if the opportunity you pursue is in another country.
Foreign residency limitations benefit disability insurance companies in several ways. By requiring you to remain mostly in the country while receiving benefits, these limitations simplify the payment process and reduce the possibility that insurers will need to communicate with doctors in other countries to manage your claim. They also make it easier for insurance companies to schedule field interviews and conduct surveillance of you to find out if you have done something that could be interpreted as inconsistent with your claim.
While these limitations are not included in every disability insurance policy, it is important to check if your policy—or a policy you are considering purchasing—contains a foreign residency limitation, because it could limit your ability to collect benefits later on.
Foreign residency limitations vary by policy. Here is an example of one foreign residency limitation from a Guardian policy:
————————————————————————————————————————————
Limitation While Outside the United States or Canada
You must be living full time in the 50 United States of America, the District of Columbia or Canada in order to receive benefits under the Policy, except for incidental travel or vacation, otherwise benefits will cease. Incidental travel or vacation means being outside of the 50 United States of America, the District of Columbia or Canada for not more than two non-consecutive months in a 12-month period. You may not recover benefits that have ceased pursuant to this limitation.
If benefits under the Policy have ceased pursuant to this limitation and You return to the 50 United States of America, the District of Columbia or Canada, You may become eligible to resume receiving benefits under the Policy. You must satisfy all terms and conditions of the Policy in order to be eligible to resume receiving benefits under the Policy.
If You remain outside of the 50 United States of America, the District of Columbia or Canada, premiums will become due beginning six months after benefits cease.
————————————————————————————————————————————
This limitation highlights several details you should look for if your disability policy contains a foreign residency limitation, including the length of time you can spend in another country before your insurance company will suspend your disability benefits, whether you can resume receiving disability benefits if you return to the country, and when you will have to resume paying premiums if your insurance company suspends your disability benefits. Another important consideration is the effect a foreign residency limitation will have on your policy’s waiver of premium provision. Under the policy above, premiums will continue to be waived for six months after benefits are suspended. However, your disability insurance policy may have a different requirement regarding payment of premiums, so it’s important to read your policy carefully.
Here is an example of another foreign residency limitation from a different Guardian policy:
————————————————————————————————————————————
Foreign Residency Limitation
We will not pay benefits for more than twelve months during the lifetime of this policy when you are not a resident of the United States or Canada.
————————————————————————————————————————————
This limitation contains much less detail than the first limitation. For instance, it does not clarify how suspension of disability benefits will affect waiver of premium. If your disability policy contains a foreign residency limitation that does not discuss waiver of premium, you should look to your policy’s waiver of premium provision to find out when premiums will become due after disability benefits are suspended. The policy above also defines foreign residency differently than the first policy. At first glance, it may seem that you can continue to receive disability benefits any time you leave the country for twelve months or less. What the policy actually says, though, is that the insurance company will only pay benefits for twelve months that you are out of the country at any time you are covered by the policy. So, if you have received disability benefits for twelve months while living in another country—even if those months were spread out over several years—your insurance company will not pay benefits in the future unless you are in the United States or Canada.
As you can see, foreign residency limitations vary among disability policies. If you are thinking about leaving the country, it is important to read your disability insurance policy carefully first so that you understand how leaving the country may affect your ability to recover disability benefits.






